A mastectomy can affect your shoulders, neck, and upper back years down the road –Physical Therapy can help avoid both the general pain and disabling shoulder pain afterwards.
Physical Therapy is an important component and is often missed in the treatment of breast cancer patients. Studies have shown, even years after a mastectomy, individuals can develop compensatory movement and posture of the shoulder blade muscles. This can lead to shoulder pain, or in more extreme cases, adhesive capsulitis (frozen shoulder). Patients can also develop irreversible nerve damage, which can cause discomfort to the cervical spine or neck. These symptoms of pain, immobility, and strength deficits can reduce quality of life long after the cancer treatments have ended.
Mastectomy pain is often the result of scarring and adhesion formation that occurs to help the body heal after radiation or surgery. Adhesions that persist after a mastectomy can cause disabling pain and dysfunction in the neck and upper back.
Women who have healed their superficial scars can have pain at the surgical scar, throughout the chest wall, and into the shoulders or arms without symptoms of significant lymphedema being present. Mild to severe symptoms of tightness can occur, often feeling like a straightjacket across the chest wall. This could affect the manner in which someone breathes, further affecting posture and abdominal muscle recruitment patterns (core strength).
Common complications that physical therapy can address:
- Scar tissue and adhesions to avoid stiff joints movement and postural restrictions.
- Swelling – surgical treatment or radiation can disrupt lymphatic circulation and cause a buildup of protein rich fluid resulting in lymphedema. This may cause heaviness and fatigue or tingling sensations in the limb and can be addressed by a therapist trained in lymphedema treatment called manual lymph drainage.
- Nerve symptoms – scar tissue and postural guarding with muscle spasm can cause impinge upon nerves resulting in significant pain. Physical Therapy can relieve symptoms related to this
- Muscle weakness/deconditioning – post cancer treatment muscle weakness can cause postural changes that can affect the shoulder area. A Physical Therapist will evaluate and treat this.
- Radiation fibrosis – causes deep scarring which creates decreased movement and tightness of the joints. This can affect posture in the long term and can also compromise lymphatic circulation.
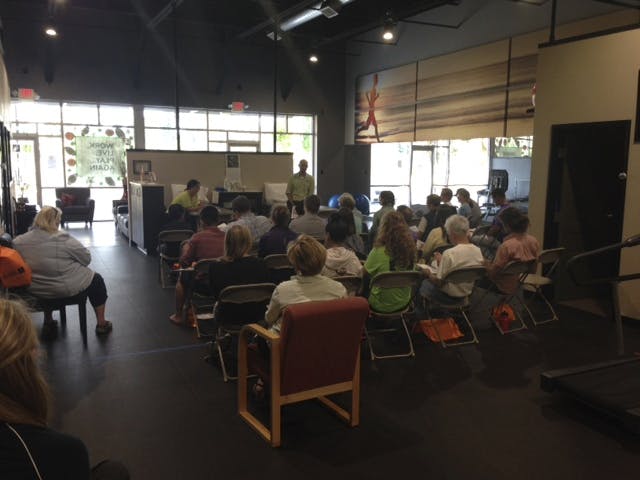
Physical therapy treatment can assist in reducing the myofascial adhesions, restoring nerve mobility and restoring normal breathing and movement patterns. These improvements lead breast cancer survivors back to live, work, and play again.
– Carrol Esterhuizen, PT, DPT, MHS, OCS, CPI


 or headaches. Take a look at this picture – what do you look like when you’re on the phone?
or headaches. Take a look at this picture – what do you look like when you’re on the phone?